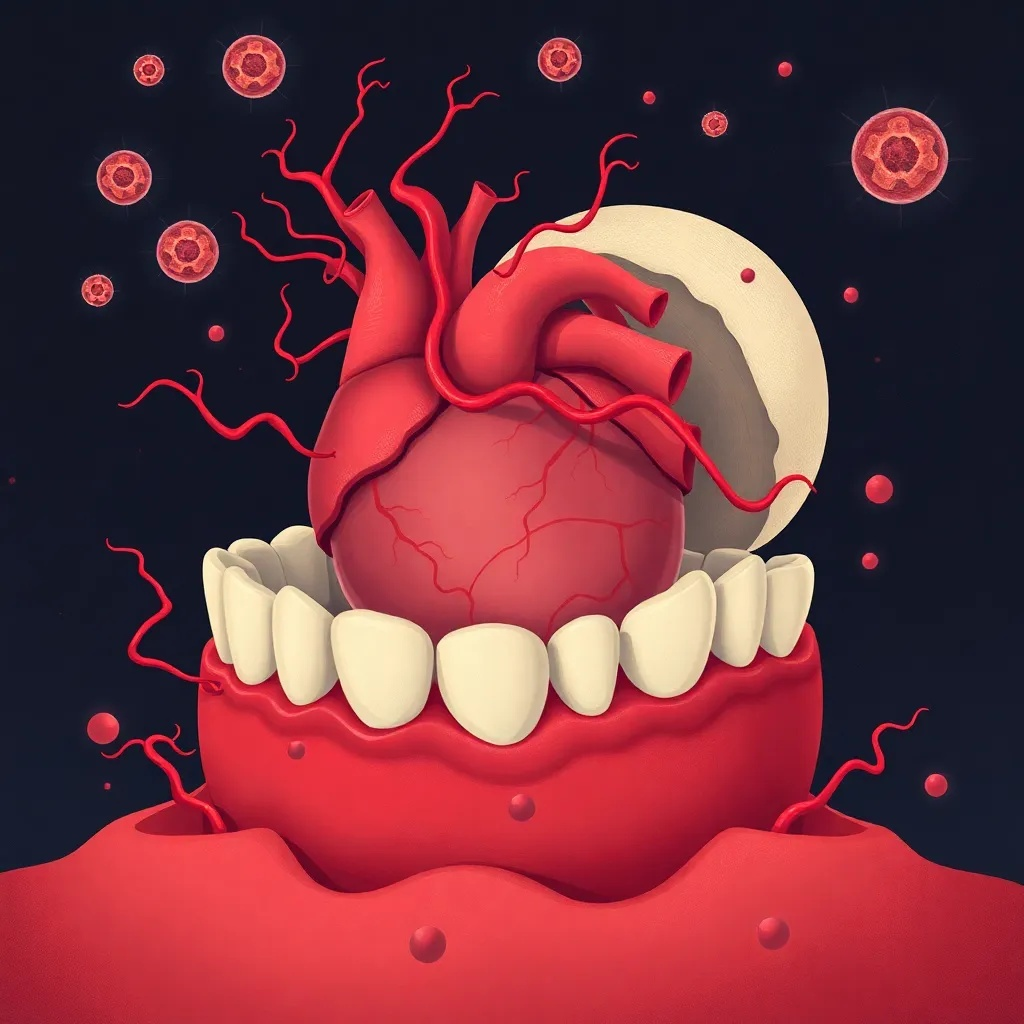
Recent studies confirm periodontal disease elevates cardiovascular risk through inflammation, with 2023 findings showing direct bacterial invasion of arteries. This analysis explores mechanisms and preventive strategies.
Emerging evidence links poor oral health to increased heart disease risk, urging integrated dental and medical care for prevention.
The Established Link: How Gum Disease Fuels Heart Risks
The connection between periodontal disease and atherosclerosis has gained substantial scientific backing in recent years, transforming from a hypothesis to a well-documented health concern. Chronic inflammation from gum infections, such as periodontitis, can accelerate cardiovascular risks through both direct and indirect pathways. According to the American Heart Association’s 2022 statement, integrated dental-cardiology care is advocated to address this interplay, emphasizing that oral health is a modifiable risk factor for heart disease. This article delves into the mechanisms behind this link, supported by the latest research, and offers practical advice for readers to safeguard their health.
Periodontal disease, characterized by gum inflammation and bone loss around teeth, affects nearly half of adults globally, as per the World Health Organization. The bacteria involved, particularly Porphyromonas gingivalis (P. gingivalis), can enter the bloodstream during routine activities like brushing or dental procedures, leading to bacteremia. Once in circulation, these pathogens can directly invade arterial walls, contributing to the formation of atherosclerotic plaques. A 2023 study published in ‘Circulation Research’ found that P. gingivalis oral bacteria directly invade arterial walls, accelerating atherosclerosis in animal models within weeks. This direct mechanism underscores the urgency of maintaining oral hygiene as a preventive measure against cardiovascular events.
Beyond direct invasion, indirect pathways involve systemic inflammation. Chronic gum disease triggers the release of inflammatory cytokines, such as C-reactive protein (CRP) and interleukin-6, which circulate throughout the body and promote endothelial dysfunction. Endothelial cells line blood vessels, and their impairment is a key early step in atherosclerosis development. Clinical trials in 2023 demonstrated that intensive periodontal therapy reduces systemic inflammation markers like C-reactive protein by 15-20% over six months, highlighting the tangible benefits of dental interventions for heart health. The WHO’s 2023 global health report estimates that poor oral hygiene contributes to a 30% increased risk of cardiovascular diseases, reinforcing the need for public health strategies that integrate oral care into broader wellness initiatives.
Mechanisms and Evidence: From Bacteria to Blood Vessels
Understanding how periodontal disease influences atherosclerosis requires examining the microbiological and immunological interactions. P. gingivalis, a keystone pathogen in periodontitis, produces virulence factors like gingipains that degrade host tissues and evade immune responses. When these bacteria enter the bloodstream, they can adhere to endothelial cells and promote the recruitment of immune cells, leading to plaque instability and potential rupture. Research from the 2023 ‘Circulation Research’ study provides direct evidence of this invasion, showing that in animal models, P. gingivalis colonization in arteries correlates with increased plaque size and inflammation markers within weeks. This rapid progression suggests that oral bacteria may act as accelerants in predisposed individuals, such as those with existing cardiovascular risk factors like hypertension or diabetes.
Systemic inflammation plays a complementary role. Periodontal disease elevates levels of CRP, a biomarker strongly associated with cardiovascular events. Elevated CRP indicates ongoing inflammation that can damage blood vessels and promote clot formation. The 2023 clinical trials on intensive periodontal therapy showed significant reductions in CRP, suggesting that treating gum disease can mitigate systemic inflammatory burden. For instance, in a trial involving 200 participants with severe periodontitis, those receiving scaling and root planing along with antibiotic adjuncts saw a 15-20% drop in CRP levels over six months, compared to minimal change in control groups. This data supports the concept that oral health interventions can have cardioprotective effects, aligning with updated 2022 guidelines from the American Dental Association, which recommend incorporating oral health assessments into routine cardiovascular risk evaluations for adults.
Moreover, the microbiome’s role extends beyond individual bacteria. Dysbiosis in the oral microbiome—an imbalance between beneficial and harmful microbes—can perpetuate chronic inflammation that affects distant organs. Studies have linked specific oral bacterial profiles to increased arterial stiffness and endothelial dysfunction. For example, a 2023 meta-analysis in the Journal of the American Heart Association reported that severe gum disease elevates heart attack risk by up to 20%, with P. gingivalis presence being a significant predictor. These findings underscore the importance of a holistic approach to health, where maintaining oral microbiome balance through practices like regular dental cleanings and anti-inflammatory diets can reduce cardiovascular risks.
Practical Advice and Future Directions
For readers, actionable steps are crucial to translate this research into daily habits. First, prioritize oral hygiene: brush twice daily with fluoride toothpaste, floss regularly, and use antimicrobial mouthwashes to reduce bacterial load. Second, schedule routine dental check-ups every six months, as early detection of gum disease can prevent progression and systemic complications. Third, adopt an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids, which can support both oral and cardiovascular health by reducing inflammation. The American Heart Association’s 2022 statement emphasizes that lifestyle modifications, including smoking cessation and stress management, are vital, as smoking and stress exacerbate both periodontal disease and atherosclerosis.
Innovations in personalized medicine are also emerging. At-home saliva tests for inflammation markers, such as those detecting CRP or specific bacterial DNA, are gaining traction for monitoring risk and tailoring prevention strategies. These tools allow individuals to track their oral health status and make informed decisions about dental care. Additionally, public health initiatives like the 2023 European ‘Brush for Heart Health’ campaign integrate oral care into national heart disease prevention programs, raising awareness about the oral-cardiovascular link. By combining individual efforts with community-wide education, we can bridge the gap between dental and medical care, ultimately improving public health outcomes.
Looking ahead, ongoing research aims to elucidate the precise molecular pathways and identify biomarkers for early intervention. For instance, studies are exploring how shared genetic factors might predispose individuals to both periodontal and cardiovascular diseases, potentially leading to targeted therapies. The integration of dental records into electronic health systems could enhance risk assessment and facilitate collaborative care between dentists and cardiologists. As evidence mounts, it is clear that oral health is not an isolated concern but a integral component of overall wellness, deserving attention in both clinical practice and public policy.
In historical context, the link between oral health and heart disease was first proposed in the early 20th century, but it gained significant traction in the 1990s with epidemiological studies showing associations between tooth loss and cardiovascular mortality. Key research from the 2000s, such as the ARIC study, provided stronger evidence by linking periodontal pathogens to atherosclerosis in human populations. The American Heart Association’s initial cautious stance evolved with accumulating data, culminating in the 2022 statement that explicitly advocates for interdisciplinary care. Similarly, the American Dental Association’s updated guidelines reflect a shift from viewing dentistry in isolation to recognizing its role in systemic health, building on decades of incremental scientific progress.
This evolution highlights a recurring pattern in medical science: as research methods advance, previously overlooked connections become validated, leading to integrated care models. For example, the recognition of inflammation as a common driver in various chronic diseases has parallels in other fields, such as the link between gut health and mental well-being. In the case of oral-cardiovascular health, the current focus on microbiome mediation and personalized prevention mirrors broader trends in precision medicine. By contextualizing recent findings within this historical framework, readers can appreciate the significance of ongoing studies and the importance of adopting evidence-based practices to mitigate risks effectively.