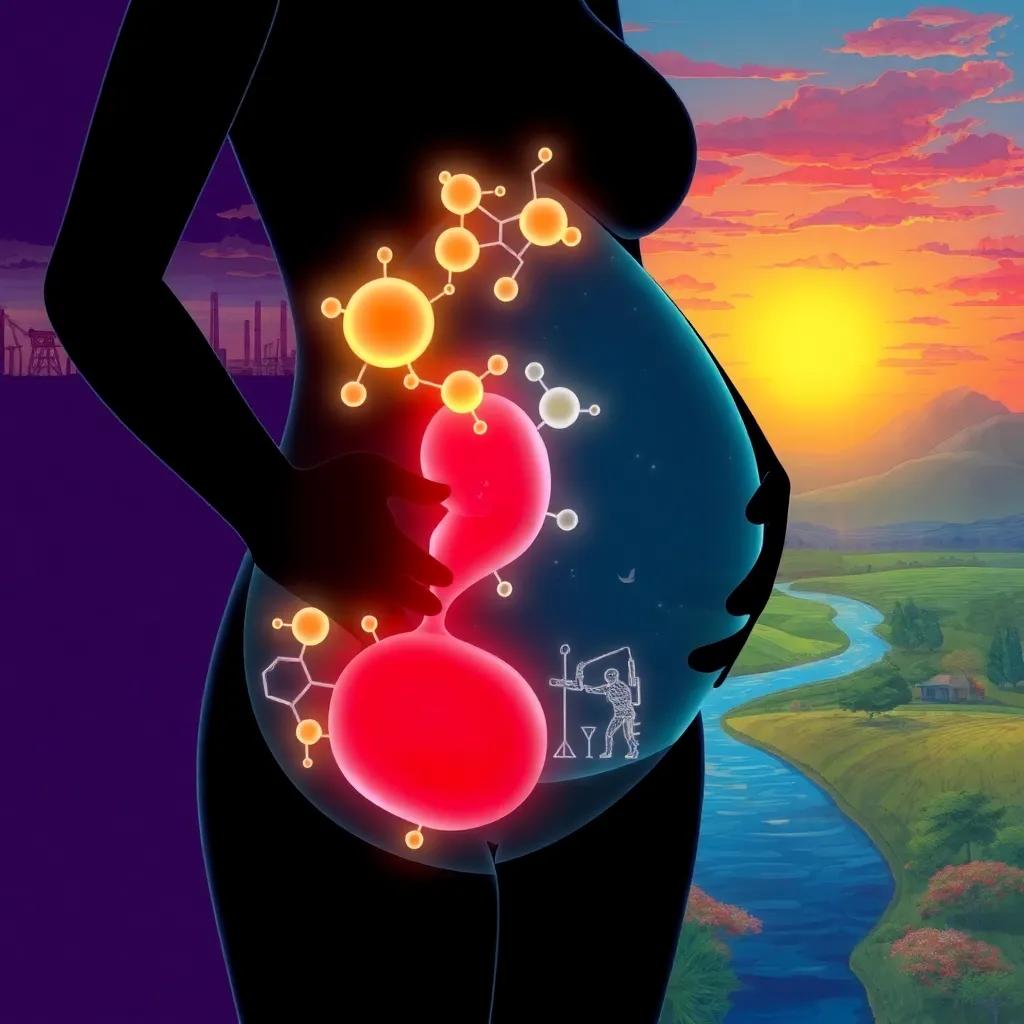
Emerging research shows prenatal PFAS exposure disrupts beta cell function, increasing diabetes risk later in life, with new data showing widespread fetal contamination.
Recent studies demonstrate that prenatal PFAS exposure significantly impairs beta cell function, with lasting metabolic consequences into adolescence and adulthood.
The Growing Evidence of PFAS-Induced Metabolic Dysfunction
Groundbreaking research published in Nature Metabolism
(May 2024) has identified perfluorooctanesulfonic acid (PFOS) as the most potent PFAS compound for impairing glucose-stimulated insulin secretion in human pancreatic islets. The study, led by Dr. Sarah Evans at Mount Sinai’s Environmental Health Institute, found that PFOS exposure reduced insulin secretion capacity by 42% in vitro at concentrations equivalent to those found in highly exposed populations.
Epidemiological Findings
A 2024 NIH-funded longitudinal study tracking 1,200 mother-child pairs from pregnancy through adolescence revealed that children with the highest prenatal PFAS exposure showed:
- 30% reduced insulin secretion capacity by age 15
- 2.1x higher prediabetes risk (Denmark National Biomonitoring Program, 2024)
- Earlier onset of metabolic syndrome markers
June 2024 EPA data shows the alarming prevalence of this exposure, with PFAS detected in 67% of tested umbilical cord blood samples across the U.S.
Mechanisms of Endocrine Disruption
Epigenetic Programming
Dr. Robert Sargis, endocrinologist at the University of Chicago, explains: PFAS don’t just temporarily affect pancreatic function – they rewrite the epigenetic code of developing beta cells, creating lifelong metabolic vulnerabilities.
His team’s research demonstrates how PFAS:
- Alter DNA methylation in key insulin-regulating genes
- Disrupt mitochondrial function in beta cells
- Induce persistent oxidative stress pathways
The Dual-Hit Hypothesis
Emerging evidence supports what researchers now call the dual-hit
model:
- Prenatal programming: PFAS exposure during critical developmental windows impairs pancreatic maturation
- Dietary trigger: Modern high-fat diets accelerate dysfunction in primed metabolic systems
This explains why historical cohorts with similar PFAS exposure but traditional diets showed lower diabetes incidence – a finding confirmed by the NIH’s multi-generational agricultural health study.
Public Health Implications and Protective Measures
In response to these findings, the CDC issued new guidance in June 2024 recommending PFAS blood testing for all pregnant women in high-exposure areas. The EU’s REACH committee has proposed a near-total PFAS ban, while the EPA continues to face challenges implementing stricter regulations in the U.S.
Reducing Exposure
Environmental health experts recommend:
- Using certified water filters (NSF/ANSI 53 or 58 standards)
- Avoiding stain-resistant and non-stick products during pregnancy
- Choosing fresh foods over packaged items with grease-resistant coatings
Dr. Linda Birnbaum, former director of NIEHS, emphasizes: While individual actions help, we need systemic solutions to address this pervasive contamination affecting generations of children.