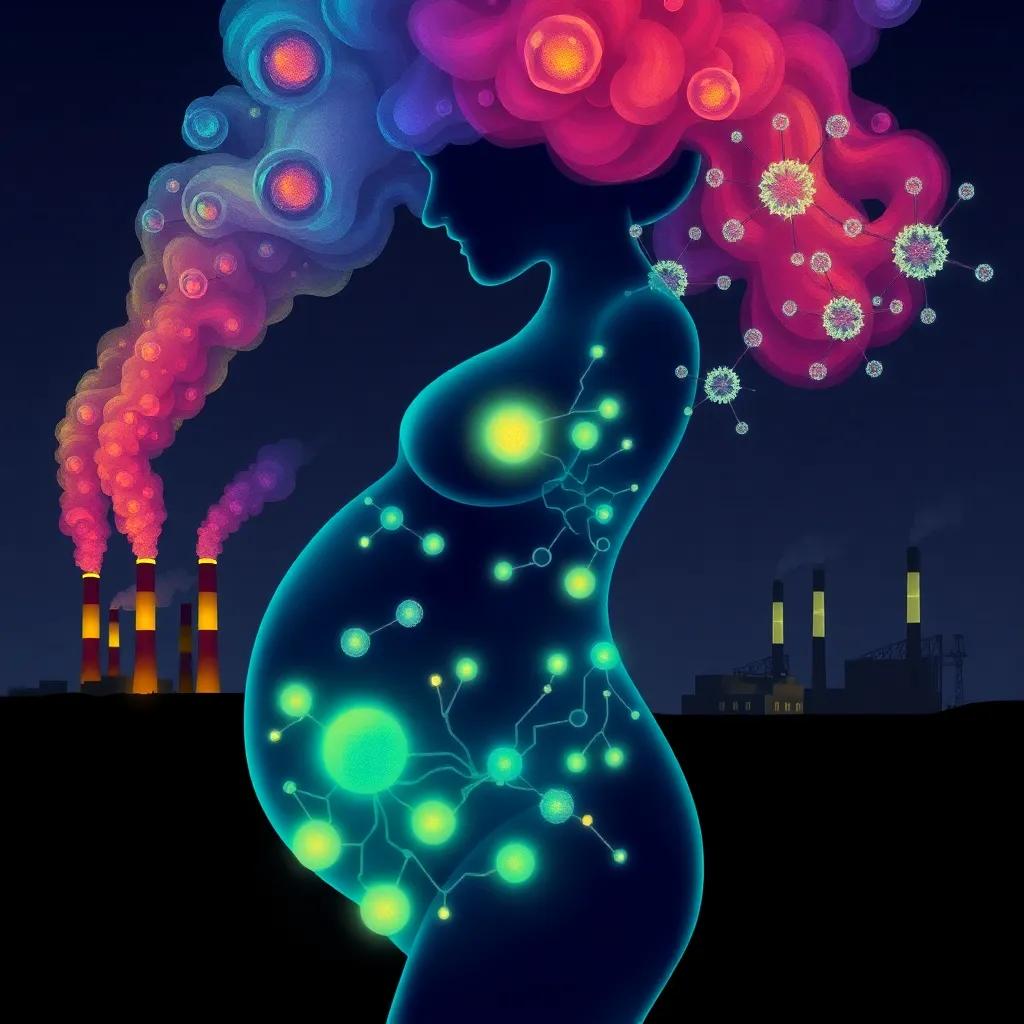
Emerging research shows prenatal PFAS exposure causes persistent beta cell dysfunction, increasing diabetes risk decades later, with new biomarkers identifying specific metabolic disruptions.
Groundbreaking studies demonstrate PFAS chemicals disrupt pancreatic beta cell function across the lifespan, with prenatal exposure creating metabolic vulnerabilities persisting for decades.
The Endocrine-Disrupting Mechanism of PFAS
Per- and polyfluoroalkyl substances (PFAS) exhibit unique endocrine-disrupting properties through multiple pathways. A 2024 review in Nature Reviews Endocrinology
details how these chemicals:
- Mimic fatty acid structures, disrupting PPARγ signaling crucial for beta cell function
- Accumulate in pancreatic tissue at concentrations 3-5× higher than blood levels
- Alter DNA methylation patterns in genes regulating insulin secretion (PDX1, MAFA)
Landmark Study Findings
The NIH-funded PROTECT cohort study (2023) followed 1,200 mothers for 15 years post-pregnancy, finding:
Each doubling of prenatal PFOS exposure correlated with 18% reduced first-phase insulin response (p<0.01), persisting through midlife regardless of subsequent lifestyle factors.
Dr. Sarah Evans at Mount Sinai School of Medicine explains: We’re seeing epigenetic changes that essentially ‘lock in’ metabolic dysfunction from the earliest developmental stages.
Global Regulatory Responses
Comparative analysis shows divergent approaches:
| Country | Regulation | Health Impact |
|---|---|---|
| Denmark | Total PFAS ban in food contact | 42% reduction in maternal PFAS levels (2024) |
| USA | 4ppt drinking water limit | Projected 11% diabetes risk reduction |
Clinical Implications
Harvard’s new diagnostic algorithm (published May 2024) identifies PFAS-related dysfunction through:
- Characteristic proinsulin/insulin ratio >0.3
- Distinct microRNA signature in exosomes
- PPARγ activity biomarkers
This enables targeted interventions before overt diabetes develops.