The vagus nerve is vital for emotional and physical well-being. Learn proven methods, supported by research, to enhance vagal tone and promote relaxation.
Understanding how vagal tone influences daily life can open new pathways to better health, including reduced stress and improved emotional resilience in the face of challenges.
Introduction: The Central Role of the Vagus Nerve
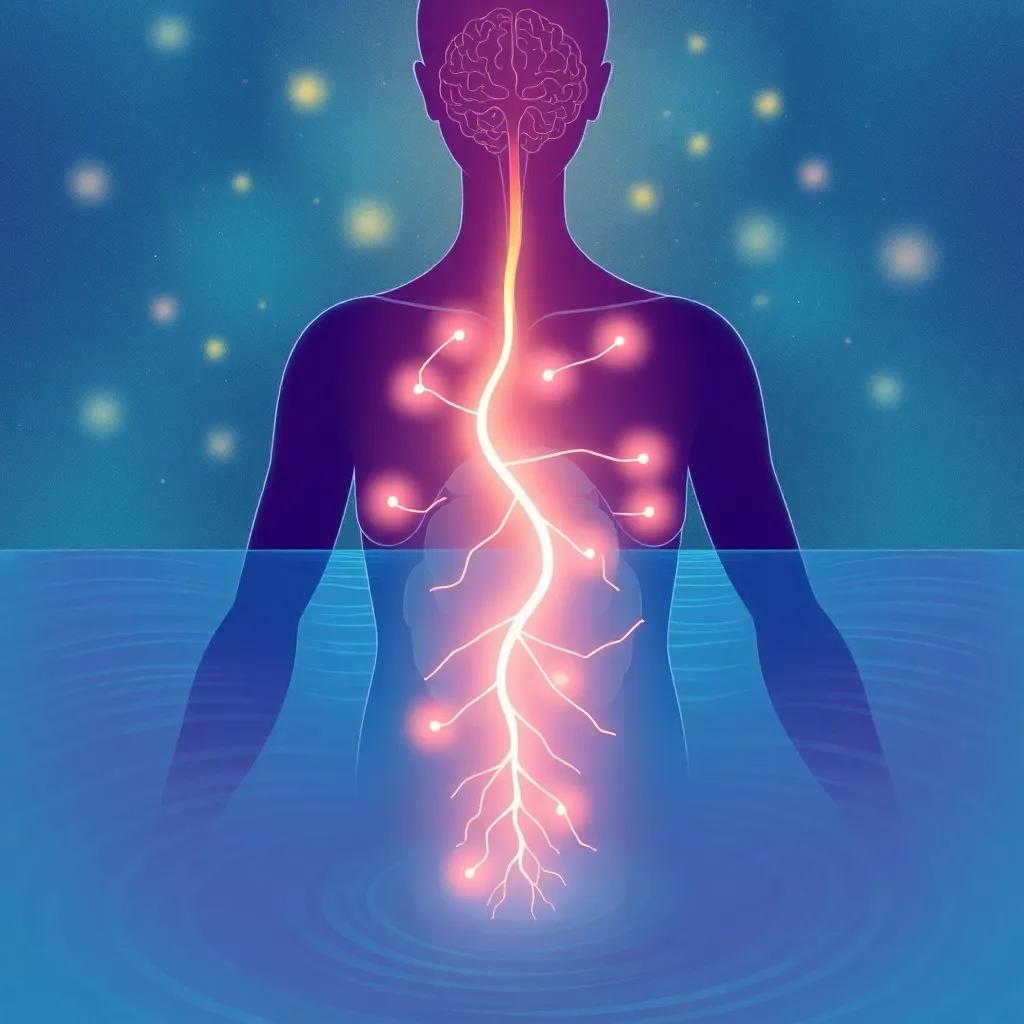
The vagus nerve is more prominent in everyday health than many people realize. As the 10th cranial nerve, it extends from the medulla oblongata in the brainstem through the neck, chest, and abdomen, influencing multiple organ systems along the way. This includes the heart, lungs, and gastrointestinal tract. Often referred to as the wandering nerve
, it helps govern relaxation responses, digestion, heart rate, and various involuntary processes crucial for survival. The key to its widespread influence lies in its function within the parasympathetic nervous system, commonly known as the “rest and digest” branch of the autonomic nervous system.
High-quality peer-reviewed studies cataloged on PubMed link robust vagal function to many benefits, including reduced inflammation, improved mood, and enhanced stress resilience. By contrast, low vagal tone often correlates with heightened stress responses and systemic imbalances. Fostering a healthy vagus nerve, therefore, becomes a strategic approach to maintaining a balanced mind-body connection.
In this article, we will delve deep into the tactics that can help optimize vagal tone and, in turn, contribute to greater psychological and physical well-being. We’ll explore evidence-based practices—such as specific breathing exercises, mindful meditation, nutritional changes, and physical activity routines—that engage the vagus nerve. Through these simple but powerful techniques, you may discover a compelling route to better emotional resilience, stable immune responses, and holistic health.
Understanding the vagus nerve’s function may seem technical, but it is vital for anyone interested in holistic or integrative health. Whether you’re a physician looking to integrate new approaches into clinical practice or an individual seeking natural ways to cut stress, the information provided can serve as a valuable toolset. This journey begins with learning about what the vagus nerve actually does and why it is so pivotal to the body’s overarching systems.
Anatomy and Function of the Vagus Nerve
The vagus nerve originates in the brainstem within the medulla oblongata region. From there, it travels downward through the jugular foramen in the skull, branching out to innervate numerous organs in the neck, thorax, and abdomen. This includes the larynx, esophagus, heart, lungs, and digestive tract. Due to its extensive reach, the vagus nerve is recognized as a prime communication highway, carrying signals that regulate activities like swallowing, speech, breath control, and even certain reflexes such as gagging and coughing.
When functioning optimally, the vagus nerve plays a key role in the parasympathetic nervous system, which helps the body manage rest, repair, and digestion. In effect, a well-toned vagus nerve counters the effects of the sympathetic “fight or flight” response, bringing the body back to a balanced state after stressful events. This capacity to recover from stress is one of the hallmarks researchers look at when studying resiliency and mental health outcomes.
Peer-reviewed data from PubMed and other reputable medical journals demonstrate that high vagal tone can correlate with reduced levels of stress hormones like cortisol. Furthermore, those with stronger parasympathetic regulation often present with more stable mood profiles, lower risk of cardiovascular events, and healthier inflammatory markers. This multi-faceted role underscores the importance of understanding the anatomical structure and the physiological function of the vagus nerve if we aim to harness its benefits for both mental and physical health.
On the other hand, an underactive or poorly regulated vagus nerve may lead to symptoms like chronic stress, gastrointestinal problems, and an exaggerated response to mental or emotional triggers. By being mindful of vagus nerve health, individuals can spot potential signs of autonomic imbalance sooner, often allowing for timely lifestyle interventions or medical advice. This perspective encourages practitioners and patients alike to pay attention to neurophysiological signals and consider them as key indicators of overall health.
In short, from monitoring heart rate
to facilitating digestion
, the vagus nerve is a conductor of the body’s internal symphony. Its tone, or operational strength, not only shapes our stress responses but also orchestrates a variety of biological processes that together promote a sense of well-being. Next, we’ll delve into the concept of vagal tone in more detail, examining why it is measured and how it factors into current medical research and clinical practice.
Understanding Vagal Tone and Its Measurement
Vagal tone, in broad terms, refers to how effectively the vagus nerve carries out its regulatory functions. One of the most widely referenced ways to gauge vagal tone is through heart rate variability (HRV), a measure of the variation in time intervals between heartbeats. A higher HRV often signifies a robust ability to adapt to stress, while a lower HRV can indicate rigid stress responses and reduced parasympathetic function.
Researchers emphasize HRV because it captures the interplay between the sympathetic and parasympathetic divisions of the autonomic nervous system. In real-world terms, when you are calm and your breathing is regular, your parasympathetic system exerts a greater influence. This triggers signals via the vagus nerve that slow down the heart rate slightly during exhalation, leading to an appreciable fluctuation in heartbeats. Consequently, a flattened HRV—meaning little fluctuation—could be a sign that the body struggles with stress adaptation, potentially leading to chronic tension, anxiety, or even immune dysregulation.
Beyond HRV, clinical assessments of vagal tone sometimes incorporate tests of the gastrointestinal function or even psychological inventories to examine stress-processing patterns. For instance, individuals with well-maintained vagus function might bounce back faster from negative emotional states or show improved emotional stability over time. These observations align with findings from programs endorsed by major health organizations. For example, strong vagal function is associated with improved resilience
in the face of trauma or burnout, as described in multiple research papers archived by recognized medical bodies.
Understanding these measurements is not merely theoretical—real-world applications abound. Wearable devices that estimate HRV, as well as specialized clinical tools, can help individuals monitor their progress in real-time. By tracking changes in vagal activity, people gain a clearer picture of how lifestyle modifications—like altered diet or a new breathing routine—may influence their stress thresholds. This kind of feedback can encourage consistent adherence to healthy practices, forming a feedback loop that strengthens overall well-being.
Crucially, though, these measurements are just one piece in the health puzzle. Individual biology, mental state, and environmental conditions all shape vagal function. Recognizing this nuance helps practitioners and patients adopt a more comprehensive approach—one that combines lifestyle strategies, mind-body techniques, and potentially targeted medical interventions. Let’s explore the well-documented techniques that specifically stimulate the vagus nerve and enhance parasympathetic functions.
Techniques to Stimulate the Vagus Nerve
Several evidence-backed methods can support vagal tone, and they vary in complexity from the very simple—like controlled breathing—to the more structured, such as regular meditation and specific cold-exposure protocols. Integrating these techniques into a daily routine can create a supportive environment for the parasympathetic nervous system to flourish.
Deep Breathing Protocols: One of the most accessible ways to stimulate the vagus nerve is through slow, controlled breathing that emphasizes the exhalation. For instance, breathing in for a count of four, then exhaling for a count of six or eight, can boost parasympathetic activity. According to reports referenced by the American Psychological Association, mindful breathing routines are consistently linked to lowered stress markers
. These techniques help the heart rate slow down, encouraging vagal engagement and promoting calmness.
Meditation and Mindfulness Practices: Studies on meditation, including loving-kindness meditation, show a positive correlation with improved vagal tone. The notion behind meditation is that deliberate focus on the present moment calms racing thoughts
and reduces tension in the body. Regular practice can, over time, raise baseline parasympathetic activity, aiding in daily stress management.
Singing, Humming, Gargling: Although sometimes overlooked, mechanical stimulation of the throat and vocal cords can influence branches of the vagus nerve. Activities such as humming or chanting create vibrations that resonate within the throat area, gently activating the nerve. Even something as mundane as gargling with water can create a mild stimulation that, when done consistently, might help support parasympathetic function.
Cold Exposure: In recent years, there has been an upsurge in discussions about the benefits of cold therapy. Some controlled research suggests that short bursts of cold exposure—e.g., cold showers or brief ice baths—can trigger a parasympathetic rebound. This phenomenon occurs as the body naturally attempts to restore thermal equilibrium, thus temporarily boosting vagal tone and possibly fostering resilience to stress over time.
These methods share a unifying theme: they aim to reduce excessive sympathetic overdrive and enhance parasympathetic control. While each technique differs in style, they all strive for a common goal: helping the body shift from a stress-dominant state to one of relaxation and restoration. Incorporating one or more of these interventions may lead to tangible improvements in mood, energy, and physical health, though individuals should tailor their approach to their unique needs and possibly consult a healthcare professional for guidance.
Lifestyle Strategies that Support Vagal Health
Beyond targeted vagus nerve stimulation exercises, everyday lifestyle choices also play a vital role in long-term autonomic balance. From the food we eat to the quality of our sleep, each aspect can reinforce or undermine our body’s default rest-and-digest mode. Several research publications, including those cited by Healthline and other reputable sources, point to the cumulative power of consistent lifestyle measures in shaping overall health.
Physical Activity: Regular exercise is a cornerstone of good health. Engaging in moderate activities like yoga, walking, or swimming helps condition the heart and lungs, but it also has measurable impacts on the autonomic nervous system. According to multiple peer-reviewed studies, practitioners of low-impact exercises such as yoga often show a marked increase in heart rate variability and better emotional regulation. It appears that the structured breathing and gentle muscle engagement in these exercises can promote parasympathetic dominance, thereby enhancing vagal tone.
Balanced Nutrition: A healthy gut supports a healthy mind
is a phrase commonly encountered in integrative medicine. Emerging research underlines the importance of a diet that is anti-inflammatory and supports gut microbiota diversity for optimal vagal function. Foods rich in fiber—such as vegetables, fruits, and whole grains—encourage a robust gut environment. Fermented products (like yogurt, kefir, or kimchi) can introduce beneficial bacteria, potentially boosting gut-brain communication through the vagus nerve. While not a cure-all, focusing on nutrition can complement other vagal-stimulating practices, including mindful breathing or meditation.
Sleep Optimization: The link between poor sleep and heightened sympathetic activity is well-documented. Inadequate or fragmented sleep can drive up stress hormones, lowering vagal tone over time. Conversely, consistent and restful sleep patterns may help reinforce parasympathetic dominance during restorative nighttime processes. Experts often suggest creating a sleep-friendly environment by regulating room temperature, minimizing light exposure, and adhering to a regular bedtime. Combined with stress management techniques, quality sleep can make a significant difference in how well the vagus nerve performs.
Social Engagement: Positive social interactions and physical touch—such as hugging a loved one—activate pathways that reduce stress and promote comfort. According to a theory known as the social engagement system, healthy social bonds may help regulate autonomic balance. Engaging conversations, community activities, and supportive relationships can all yield subtle yet profound shifts in vagal function, helping people maintain a calmer baseline even under pressure.
By weaving these habits and behaviors into one’s daily life, individuals can cultivate a robust foundation for autonomic health. Taken together, they not only strengthen the vagus nerve’s immediate functionality but also guard against the cumulative wear and tear of modern stressors. However, there are also medical interventions designed to offer more direct support, particularly for those dealing with chronic conditions or severe stress disorders, as we will see next.
Potential Medical Interventions and Emerging Research
While lifestyle modifications and daily practice of vagal stimulation techniques are often the best first line of defense against stress, certain medical interventions have also proven beneficial. One of the more well-known approaches is vagus nerve stimulation (VNS), a procedure where an implantable device delivers electrical impulses to the vagus nerve. Clinically, VNS has been used to manage conditions like epilepsy and treatment-resistant depression, with various studies showing promising results over the past two decades.
In addition to implantable devices, researchers are exploring transcutaneous VNS (tVNS). This technique applies mild electrical stimulation to areas of the ear thought to be innervated by branches of the vagus nerve. The non-invasive nature of tVNS makes it an appealing option for broader populations who do not qualify for surgical implants. According to updates in reputable outlets, including The New York Times, several ongoing clinical trials aim to determine the optimal dosing and methodologies for these devices, as well as their potential for treating a wider range of conditions.
Moreover, mental health professionals are increasingly eyeing vagal stimulation as a supplemental tool for anxiety disorders and post-traumatic stress. While many questions remain unanswered—such as the precise long-term benefits or ideal patient populations—this cutting-edge field underscores just how malleable the vagus nerve can be under targeted interventions. The intersection of medical technology and the vagus nerve is rapidly evolving, with researchers focusing on safe, effective, user-friendly treatments of the future
.
It’s important to note, however, that these interventions are typically reserved for individuals whose conditions have not sufficiently improved through conventional therapies. Standard medical guidance often suggests optimizing basic supportive measures—physical activity, nutrition, sleep, social engagement—before considering surgical or device-based treatments. With that said, the rapid pace of innovation in this area suggests that in the coming years, vagus nerve stimulation could become a mainstream aspect of managing complex disorders ranging from autoimmune diseases to mood dysregulation.
Monitoring and Tracking Progress
One of the biggest advantages of focusing on vagal health is the relative ease of tracking progress. Wearable devices, from wrist-worn heart rate monitors to smart watches equipped with HRV tracking software, can offer quantitative insights in real time. While these tools are not always as accurate as clinical-grade equipment, they do enable a broader population to become more involved in their own health management.
Beyond technology, there is a subjective element to measuring change. Individuals often notice shifts in mood, anxiety levels, and physical energy that correlate with improved vagal tone. For example, people might find themselves recovering more quickly from stressful events and experiencing fewer headaches or digestive problems. Maintaining a simple journal to track daily habits—like diet, exercise, and meditation—and noting corresponding emotional or physical states can provide valuable feedback loops.
In clinical settings, professionals may run baseline HRV tests at the start of a therapeutic regimen and compare those to subsequent measurements following an intervention. These intervals might be spaced out over weeks or months, allowing enough time for cumulative changes to become evident. In the case of more complex issues, such as co-occurring anxiety and chronic inflammation, healthcare providers may also incorporate blood tests for inflammatory markers to gauge the indirect effects of improved parasympathetic function on overall physiology.
Whether you choose to monitor with advanced technology or simply note subjective shifts, consistent tracking can foster a solid sense of control over personal health. This process often sparks deeper motivation to maintain the daily activities that nurture the vagus nerve. Over time, seeing progress—like an uptick in HRV readings or a subjective reduction in stress—can reaffirm that small changes, practiced consistently, can have substantial impacts.
Conclusion: Embracing the Potential of Vagal Health
Improving vagal tone offers a potent avenue for bolstering both mental and physical well-being. Through an array of largely noninvasive practices—deep breathing, meditation, balanced diets, quality sleep, supportive social connections—individuals can actively cultivate a more harmonious interaction between their mind and body. Just as the vagus nerve wanders through the body, bridging critical organs with the brain, it also connects modern health science with millennia of wisdom about the power of relaxation, emotional balance, and resilience.
For those with chronic conditions or significant psychological stress, emerging medical interventions like vagus nerve stimulation offer a glimpse of innovative treatments on the horizon. However, even without advanced devices, foundational strategies exist that enable people to tap into the nerve’s calming potential. When applied consistently and conscientiously, these methods allow the parasympathetic system to shine, easing the burdens of modern life and promoting a healthier, more adaptive baseline.
Ultimately, the real strength of a well-tuned vagus nerve lies in its capacity for enduring support. By fine-tuning our inner communication
, we empower the body’s built-in healing mechanisms and psychological reserves. Readers seeking further exploration can find detailed scientific reviews on ncbi.nlm.nih.gov (PubMed), mental health studies at apa.org (The American Psychological Association), dietary guidelines on healthline.com, and regular updates on emerging medical technology from platforms like nytimes.com (The New York Times). The more we understand and harness the vagus nerve’s hidden potential, the closer we come to a more balanced and resilient existence.